*This is an article from the Spring 2024 issue of Contentment Magazine.
By Josh Briley, PhD, BCMAS, FAIS
Throughout my career as a psychologist, regardless of the setting (VA clinic, private practice, telehealth, or prison), I have struggled against the overwhelmingly common misconception that once someone begins to experience post-traumatic stress, they will always have it. That they are now somehow “broken” or “damaged” and cannot be “fixed.”
This misconception is fueled by a number of factors. One factor is the medical profession’s primary approach to psychological issues: prescribing medications. Now, while I am not anti-medication, my clinical experience has convinced me they should not necessarily be the first-line approach to overcoming post-traumatic stress. Most of the patients with post-traumatic stress that I have worked with over the years have been on psychotropic medications for sleep, anxiety, depression, and pain, with no significant improvement in their symptoms. Not only do these medications not resolve the issues contributing to the symptoms of post-traumatic stress, but they include side effects that often negatively impact the patient’s quality of life; side effects which the prescriber may address with yet another medication, and thus, the cycle perpetuates.
However, the biggest factor that keeps people “stuck” and believing they will never overcome their post-traumatic stress and that they are, therefore, somehow “broken” is a misunderstanding of what it means to “get better.” Most people I have worked with define “getting better” as forgetting about the event(s) and “going back to who I was before.” Admittedly, this is an impossible goal. We cannot go back to who we are following any significant life-changing event. For example, once you become a parent, you cannot return to thinking and acting as you did before your first child was born. Once puberty starts, you cannot go back to who you were pre-puberty. Both examples forever alter how you think, feel, and behave. Similarly, once you have experienced a traumatic event or a series of traumatic events, you will not forget it, nor will you be able to revert to thinking, acting, or feeling the way you did before the trauma(s).
Therefore, if “getting better” does not mean forgetting about the experience and going back to who you were before the trauma, then what does it mean? “Getting better” is best defined as post-traumatic growth, which involves incorporating the traumatic experience into the narrative of who you are, moving beyond the trauma reactions, and developing a new normal for your life in which you can achieve a full, happy, and healthy life without the constant emotional and physical difficulties that often keep us stuck following a trauma. The first step to attaining post-traumatic growth is to understand the reactions that occur during and following a trauma so you do not feel so out of control of yourself. Once you understand these reactions, it is essential to learn how to overcome these reactions so you can begin to experience post-traumatic growth. This article will briefly explain the reasons we react as we do following a trauma and discuss a tested but novel technology that can be utilized to help alleviate the reactions and smooth the transition to post-traumatic growth.
Physiological and Evolutionary Aspects of Post-traumatic Stress
During a traumatic experience, an aspect of the sympathetic nervous system, known as the “fight or flight” response, kicks in. Several physical and mental changes occur from this with the sole purpose of allowing us to survive a dangerous encounter. Physically, our heart rate increases, muscle tension in our arms and legs increases, breathing becomes shallower and more rapid, and blood flow is concentrated from our torso to our extremities. Mentally, we develop tunnel vision to focus on the threat and anyone in the immediate area whose safety we may feel responsible for. Higher order, logical reasoning is reduced, and our most basic experiential, emotional decision making is amplified. These changes are all designed to get us out of danger as quickly and safely as possible.
The way our nervous system is designed, once the immediate threat is over, then the parasympathetic nervous system, also known as the “rest and digest” response, is supposed to be activated to counter all of the changes from the sympathetic nervous system activation and restore us to normal functioning. In other mammals, this is precisely what happens. They encounter a threat, respond to it, and then return to normal functioning. They stay in this parasympathetic state until they encounter another danger or a reminder of the threat. At this point, they are briefly in sympathetic arousal until the new threat, or the reminder is gone.
However, unlike other mammals, humans are able to anticipate threats where there may be none and do not need a physical or situational reminder to recall the fear and heightened arousal of the trauma. Therefore, we are more prone to stay in fight or flight long-term without allowing our nervous system to return to normal.
The longer we are in a fight or flight response, the more of an effect it has on our brains and bodies. The brain is incredibly adept at becoming efficient at repetitive behaviors and emotions. Therefore, when we stay in a state of heightened arousal and look for danger everywhere, the pathways that process these threats become more active and, over time, become the default pathways for the activity in our brains. Thus, a cycle is created in which we consistently feel threats where there may be none, so our brains adapt and stay in a state of fight or flight, reinforcing the feeling of being in danger at all times. We may begin to feel as if we always have to be on alert, we may be easily startled, and our startle response may be bigger than usual. We may be prone to emotional outbursts, especially of anger, fear, or sadness, we may have difficulty relaxing and trouble falling or staying asleep. In addition, we may find ourselves reliving the trauma through either intrusive memories, nightmares, or fully re-experiencing it in the form of a flashback. As a result, we may isolate ourselves from others, have difficulty with memory or with concentrating on tasks to the extent that work and school performance suffer, and may feel easily overwhelmed.
The longer we experience these reactions to the trauma, the more entrenched the electrical pathways associated with these reactions become. In recent years, we have learned that such pathological electrical activity in the brain is associated not only with the general symptoms of anxiety, insomnia, and other difficulties often experienced as part of post-traumatic stress but the specific patterns of electrical activity can be tied to the specific difficulties a person is experiencing.
Traditional Means of Managing Post-Traumatic Stress
Because of the disruption these difficulties have on our lives, most of us go to our primary physicians and get a prescription. These medications are intended to reduce the severity of the anxiety and insomnia that occur from post-traumatic stress, and they may be able to do so for a brief period. The problem with these medications is they do not address the underlying cause for the sympathetic activation contributing to the hyperawareness and re-experiencing symptoms of post-traumatic stress. As a result, despite compliance with medications and suffering through the side effects of these medications, we do not experience significant improvement in our daily functioning. 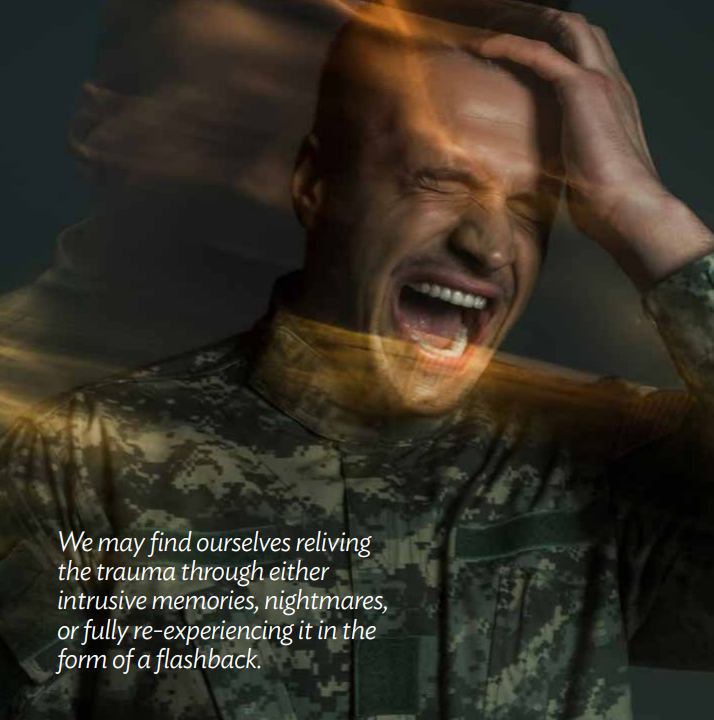
Many people also seek out therapy to help with the symptoms of post-traumatic stress. Until very recently, the most frequently utilized methods in psychotherapy to help with post-traumatic stress were treatment approaches that emphasize directly confronting the memories and triggers head-on. These are very intense treatment approaches that escalate the overwhelming and unpleasant emotions evoked by the memories of the trauma. The underlying theory of these treatment approaches is that, by deliberately recalling the avoided memories and telling the stories of what happened, we will move the memory from the intense and emotional experiential memory to the narrative memory and thus reduce the intensity of the emotional response. Therefore, sympathetic nervous activation will not be as intense, and we can move on from the trauma. When done correctly, these treatment approaches are effective, yet difficult for both patient and therapist to go through. When done incorrectly, the patient can become retraumatized, and their symptoms actually become more debilitating, leading to even more severe anxiety and insomnia.
Post-Traumatic Growth
If traditional therapy approaches and medications are often difficult or unsuccessful, then what hope does someone stuck in a post-traumatic stress cycle have? Fortunately, there is hope. It is possible, and even more accessible than many believe, for even someone with severe post-traumatic stress to move beyond these struggles. Once they learn to do so, they are no longer “stuck” in the trauma and can enjoy their life again. 
Achieving post-traumatic growth is not as impossible as it may sound. The primary component is learning to deliberately activate the parasympathetic nervous system in the face of a perceived threat or when experiencing the memory or a reminder of the trauma. There are many ways to achieve this parasympathetic activation, although a comprehensive discussion of them is beyond the scope of this article. The primary component in all of these approaches involves learning to relax the muscles in the body and learning to reframe what we tell ourselves about the trauma.
There are many ways to relax the body: progressive muscle relaxation, guided imagery, and meditation are just a few. These methods involve physically relaxing our bodies, changing our breathing patterns to a slower and deeper rhythm, and learning to focus our minds. Focusing on these physical changes can turn off sympathetic activation and activate the parasympathetic nervous system. For people who can master these skills, the results are amazing. However, many people do not have the patience, the dedication, or the time to commit to learning and practicing these skills every time they perceive danger or encounter a reminder of their trauma. Fortunately, there are technologies available that can automatically activate the parasympathetic nervous system. The most tested of these technologies is Cranial Electrotherapy Stimulation (CES).
Cranial Electrotherapy Stimulation: A Modern Approach
Cranial Electrotherapy Stimulation (CES) is a non-invasive technology that is FDA-cleared to treat anxiety and insomnia. CES, in its modern form, has been used in the United States since the early 1980s, though the roots of the technology are decades older. CES uses tiny amounts of electrical current to normalize the electrical activity in the brain. As this activity is normalized, the nervous system is essentially “reset” to operate how it is designed. The parasympathetic nervous system is automatically engaged, and relief from the anxiety that is prevalent in post-traumatic stress is often immediate and drastic. Many people describe feeling their anxiety “melt away” within a single treatment. Additionally, because the nervous system is essentially “reset” by CES, sleep quality and quantity are significantly improved. Unlike other insomnia treatments, which artificially sedate you and disrupt healthy sleep cycles, CES normalizes the electrical activity in the nervous system and improves sleep naturally. When the nervous system is operating as designed, a healthy sleep cycle is part of that operation. The results are cumulative, so the more consecutive days CES is utilized, the better the results will be and the longer they will last. While a few CES devices are on the market, the global leader in research and clinical utility is Alpha-Stim® (www.alpha-stim.com). CES is available in the United States only by a written order from a licensed healthcare provider but is available over the counter in other countries, which allows CES devices to be distributed. In Europe, Asia and most of the rest of the world, CES is approved to treat depression also, and is generally considered safe enough to not require a doctor’s order.
I have used Alpha-Stim, both as the sole method of treatment and in conjunction with therapy, to treat people struggling with chronic and often debilitating anxiety and insomnia associated with post-traumatic stress. Many of my patients had been on medications for decades, had participated in both outpatient and residential treatment, and had given up hope of having a normal life. I have worked with people who were unable to leave their houses due to the anxiety that accompanies feeling as if one is in danger everywhere they go. They isolated themselves as much as possible and, as a result, missed significant family events and had few, if any, friends. They believed they were “broken” because they did not respond to situations the way “normal” people did. Years of medications and unsuccessful attempts at therapy had convinced them they would always be that way.
However, once I introduced Alpha-Stim as a treatment modality, the differences were nothing short of remarkable. During treatments in my office, I could see them visibly relax in the chair, and many of them reported feeling better at the end of the first treatment than they had felt in years if not decades. As they obtained their own devices, they reported sleeping through the night, being able to go to the store with their spouses, attending children’s and grandchildren’s school events, and enjoying holidays with families for the first time in years. Their family members would stop me in the clinic and tell me stories of the changes they saw in my patients, often with tears in their eyes.
Inside the clinic, I also witnessed incredible transformations. Many of my patients would no longer sit along the edge of the waiting room, staring at everyone warily while waiting for an appointment. Instead, they would interact with the other patients, laughing and smiling, with no sign of anxiety. During therapy sessions, the changes were also remarkable. My patients would start their CES treatment either in the waiting room or as soon as they entered my office and were relaxed within minutes. Thus, we were able to get to the meat of the session more quickly and easily than we had before introducing Alpha-Stim, spend longer in processing the emotions and thoughts that kept them stuck in post-traumatic stress, and overcome their struggles. We could process different traumas more quickly and efficiently. As a result of the combination of CES and therapy, patients were able to overcome the difficulties that had kept them stuck and enter into a period of post-traumatic growth. Similar, though perhaps not quite as drastically, improvements were reported in patients who utilized Alpha-Stim as a sole means of treatment and did not participate in the available individual or group therapy services I provided in the clinic. Furthermore, most of the patients who used Alpha-Stim regularly were able to come off of, or at least drastically reduce the dosage of, their anxiety, depression and sleep medications.
Post-traumatic growth is not only possible; it is essential if we want to live a happy, healthy, fulfilled life. Every difficulty we encounter is an opportunity to learn more about ourselves, others, and the world. However, being stuck in a state of post-traumatic stress prevents us from moving past survival mode. Activating the parasympathetic nervous system is the most effective and efficient way of calming our minds and bodies and allowing ourselves to put the trauma into perspective and begin to rebuild our lives. CES is a very effective tool to assist in this transition and is the most effective means of facilitating the progression from post-traumatic stress to post-traumatic growth that I have used in over 20 years as a psychologist.